The Temporo-Mandibular Joint (TMJ) is a modified hinge, meaning it allows for hinging movement initially, as a person starts to open, but then gliding movement as they open further.
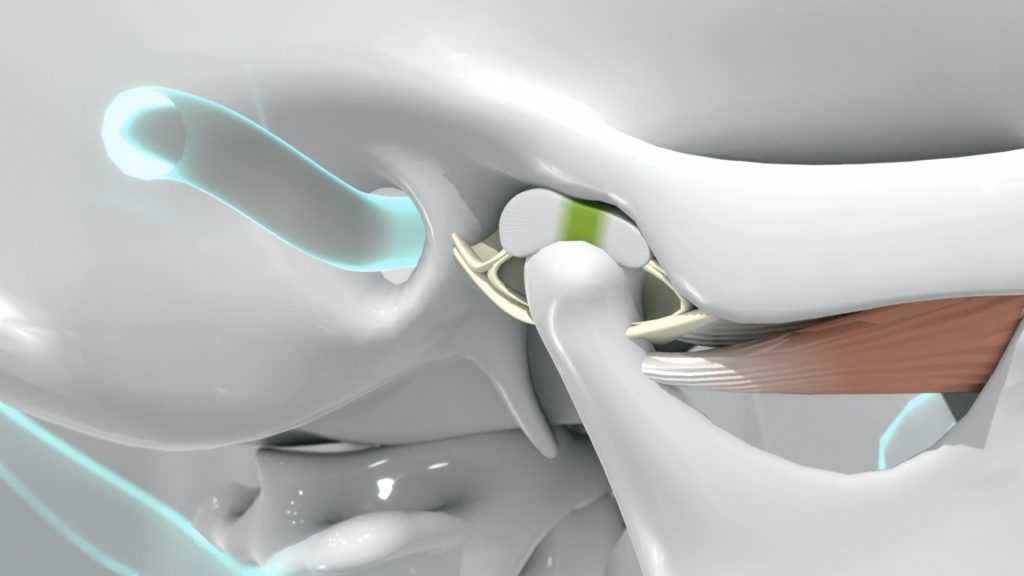
The articular surfaces of the TMJ are the mandibular fossa of the temporal bone, and the head of the mandibular condyle. A cartilage disc lies between the condyle and the fossa. This disc is very important to the TMJ because it plays a major role in stress distribution, load absorption, and lubrication of the TMJ. The articular disc can be divided into three zones according to thickness, hence the biconcave shape.
disc:
The anterior - this zone lies slightly anterior to the condyle
The intermediate - this is the thinnest portion; this zone separates the articular surface of the condyle from the slope of the articular tubercle

The posterior - this thick zone is situated between the condyle and the floor of the mandibular fossa
In the posterior zone, the disc is divided into two laminae: the superior retrodiscal lamina (elastic fibres), and the inferior retrodiscal lamina (collagen). The superior lamina attaches the disc to the tympanic plate.

In a normal healthy disc-condyle relationship, there is effective intra-articular lubrication which keeps friction to a minimum. An increase in friction can result from chronic micro trauma or acute trauma directed at the TMJ. Repetitive minor injuries occurring over a period of time cause damage and these include direct injury such as a blow to the mandible, indirect injury such as from whiplash, or simple hyperextension. Bruxism is the most common and frequent cause of micro trauma.
Studies show that the loss of posterior occlusal support is a cause of fiscal and condylar deformation and degeneration. Occlusal abnormalities also have been shown to be a fundamental factor in the onset of TMD symptoms. As a result of the micro trauma, the disc loses its viscoelastic properties and that results in thinning or perforation of the disc causing a displacement.
Disc displacement is one of the most common types of TMJ arthopathy. Some studies suggest that disc displacement precedes the onset of degenerative changes in the TMJ. Others suggest that the degenerative process predisposes the patient to disc displacement.
Disc displacement can be anterior, posterior, medial, or lateral. Movement of the disc on and off the condylar head can result in a clicking or popping sound. As long as the disc can reduce (pop back on) range of motion is not limited. When the disc can no longer reduce, this can result in limited opening, along with pain, and deviation of the mandible.
If the disc displaces posteriorly, which is rare (0.7% to 2.2% of patients with internal derangement), this results in an open lock condition, or inability for the patient to close fully. The most common clinical symptoms are: clicking followed by pain, luxation (dislocation), and open lock. Clinical signs include lack of occlusion on the affected side and deviation of the mandible. It has been found that a high prevalence of posterior disc displacement is seen in skeletal class III patients.

Treatment includes occlusal splint therapy, which is reversible and non-invasive. It helps in distributing the heavy load exerted on the articular disc during parafunction and increase the occlusal vertical dimension, usually beyond freeway space, which allows the muscles to function more efficiently during contact and be less active during postural functions. Occlusal splints decrease muscular effort resulting in relaxation of the muscles and TMJ.

