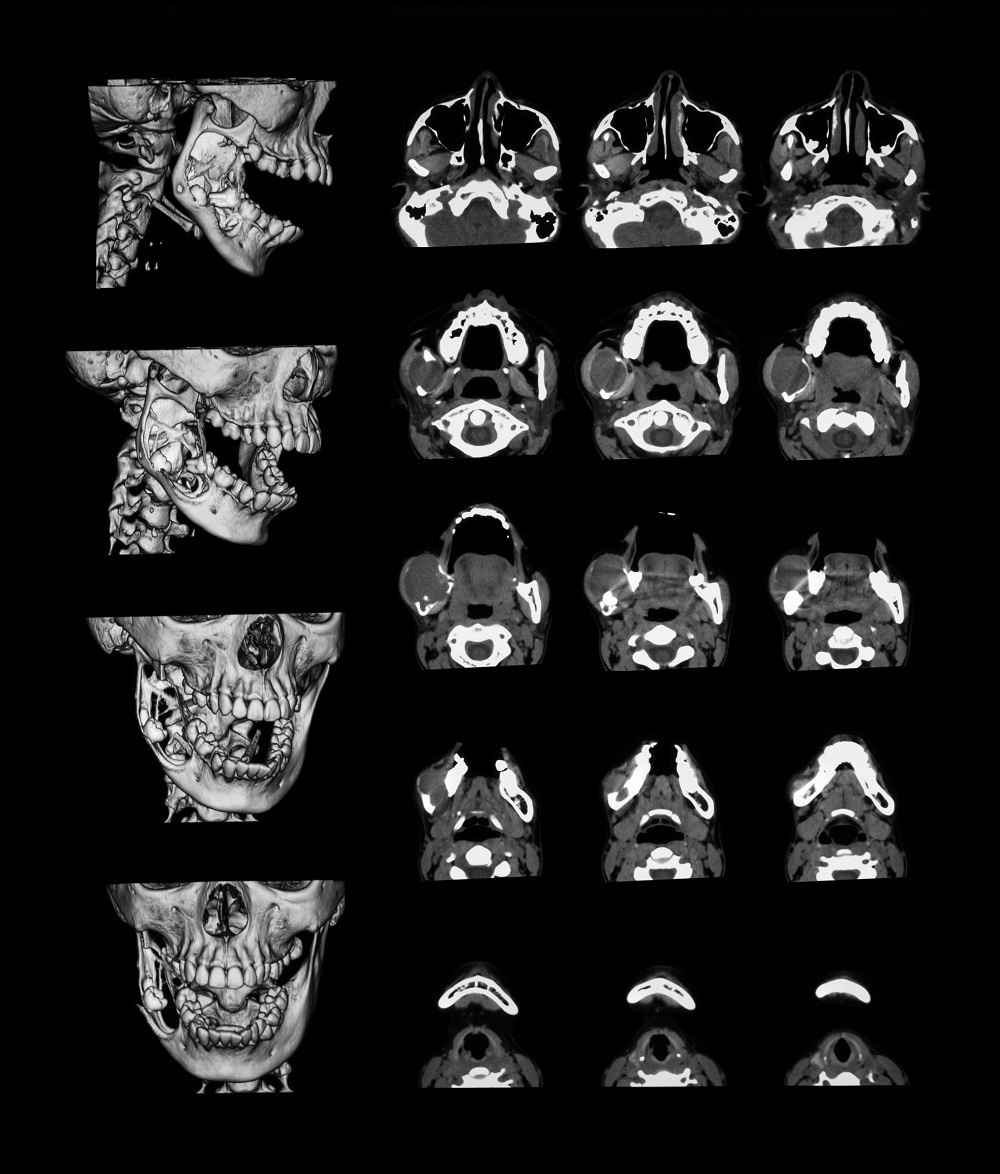
Complex, Severely Worn and Mutilated Dentition
One of the biggest challenges for dentists is treating complex cases. When dental disease is combined with lack of maintenance and allowed to go untreated for long periods of time, the resulting mutilation and irreparable damage is devastating. Studies show that nearly 1 in 5 patients over the age of 60 have no teeth. That number jumps to 1 in 3 after the age of 75. The quality of life, not to mention self-esteem, is impacted dramatically for these patients and communication and timely treatment is key to prevention. The challenge for us (dentists) is compounded by lack of proper diagnosis, inability to treatment plan all the steps required for full rehabilitation and, most importantly, communication with our patients.


It is imperative that these conditions need to be identified immediately and treated before teeth become un-restorable. Once the disease has progressed to a point where it’s visible to your eyes, it is difficult and often impossible to reverse the damage, and can result in disastrous consequences. There are multiple factors that lead to mutilated dentition, but the following are some of the most common conditions and syndromes that contribute to this :
Tooth Wear
Worn teeth don’t happen overnight. Many people are not aware that they grind their teeth when they sleep, and because the wear seems slow at first, they don’t realize the devastating effects it can lead to. Wear from grinding is one of those subtle disease processes that can sneak up on you and many people won’t think much of it until it’s way too late or extremely expensive to restore.
Gastro-Esophageal Reflux Disease (GERD)
GERD is responsible for an acid environment in the mouth. The damaging effects of acid corrosion on teeth create “Pot Hole” defects in the chewing surfaces and lead to challenges when restoring these teeth in order to manage the constant acid attack. GERD can occur in conjunction with sleep apnea, a condition that is on the rise and responsible for many health challenges.
Gum Disease
You wouldn’t think that gum (periodontal) disease could lead to this type of damage, but severe untreated periodontal disease is a major contributor to tooth loss and affects 1 in 4 adults over the age of 65.


Dry Mouth (Xerostomia)
Dry Mouth is a common condition, and can result from taking some types of prescription medications. Loss of saliva results in the loss of the “buffering” effects and results in rampant decay.
Diagnosis and Treatment of Complex Cases
Patients with complex bite or severe break-down requiring or looking to restore all or most of their teeth involve more extensive work-up and diagnostic protocols due to the complexity and challenges each individual case brings.
In order to ensure that treatment provides a beautiful and healthy restorative outcome, as well as a predictable plan for each individual step of the process, we involve a detailed diagnostic process as follows :
1. Initial Exam - the first step to a successful Restorative case is a full and comprehensive exam, which includes photos, x-rays, measurements, occlusal analysis, tooth vitality testing, periodontal assessment, and cancer screen. In addition, we may refer you to have a CBCT scan if TMJ is in question.
2. Neuromuscular Analysis - for patients who suffer from TMJ related issues, headaches, migraines, muscle pain around their head and neck, or those with severe wear or jaw misalignment, this step is invaluable to providing Dr. Bis a proper diagnosis and treatment plan in order to stabilize and resolve these issues along with restoring your teeth.
3. Photos are taken and analyzed in order to allow Dr. Bis to evaluate and resolve any soft tissue (gums) challenges, tooth shape and size, tooth position and angulation, as well as your particular desires for shade and aesthetics.
4. Occlusal Forces Bite Scan - a sensor known as the T-Scan is a tool used to restore quality of life in patients whose bite contributes to pain, discomfort, jaw misalignment, bite issues, or over-adjusted dental work. T-Scan provides dynamic occlusal (bite) measurement, revealing the level, timing, and percentage of force on individual teeth, as well as the occlusal stability of the overall bite. A T-Scan allows a visual recording, over time, that shows exactly where the teeth are touching, how bite forces are distributed, and where tooth contact is lacking, which is key to establishing a balanced, healthy, comfortable occlusion (bite).
5. Patient Education on home care and follow-up is the reason for long-term stability and success in Restorative cases. Keeping your gums and new teeth in optimal health prolongs the lifetime of your new restorations and your beautiful new smile.
